Food poisoning from food contaminated at a restaurant can be a nightmare for public health officials and result at the end of business for even a large restaurant chain. Here are some of the most notable cases of restaurant food poisoning over the last 45 years.
1977’s Trini & Carmen’s Hot Pepper Sauce

One of the earliest food poisoning cases covered by national media occurred in Pontiac, Michigan. Trini & Carmen’s was a trendy Mexican restaurant in the Detroit suburbs. In March 1977, customers reported symptoms of food poisoning. The cause was traced to homemade hot sauce using home-canned jalapeño peppers. As a result, 58 people became ill, resulting in one of the most significant botulism outbreaks in U.S. history. The restaurant was temporarily shut down, and jars of contaminated peppers were seized. No deaths were reported.
Trini and Carmen’s remains in operation today as it is still one of the most popular Mexican restaurants in the Detroit area.
1982’s E. coli. Outbreak at McDonald’s

In February through March and May through June 1982, 47 people fell ill with a rare form of E. coli after eating hamburgers at McDonald’s in Oregon and Michigan. The strain of E.coli was so rare that testing showed negative for the bacteria, and hospitals had trouble knowing how to treat the patients.
The restaurant food poisoning outbreak caused by this rare strain of E. coli resulted in published concerns over identifying bacteria that could affect the nation’s food supply and raising awareness of animals raised in concentrated animal feeding operations (CAFOs).
1993’s E.coli Outbreak With Jack in the Box Hamburgers

This E.coli outbreak by a fast food restaurant has been deemed the most infamous food poisoning outbreak in US history. In 1993, Jack-in-Box introduced a specially produced food product called the Monster Burger. Unfortunately, due to the size of the burger, it ended up in undercooked patties. In addition, the burgers were only cooked to 140 degrees F, the minimum FDA-required temperature.
The result was disastrous. Seven hundred thirty-two people were affected by E. coli. Four children died, and 178 suffered permanent kidney and brain damage. The outbreak practically bankrupted the chain and led to stronger government regulations on food handling. Improved testing by Jack-in-the-Box and the industry significantly reduced E. coli cases in fast food hamburgers.
1997 Beef Tainted by Supplier Forced Burger King to Pull Product

Burger King suffered its first significant restaurant food poisoning crisis in 1997. Then, Sixteen people suffered E.coli symptoms from the tainted hamburger. As they looked for the source of the contamination, Burger King removed all hamburgers from its menu in 650 of its 1,650 locations, selling only chicken and fish.
The source turned out to be an Arkansas-based beef processor named Hudson Food. The USDA inspected the processing facility and then summarily asked Hudson to close the facility and recall the hamburger made there in June. However, inspectors found that Hudson saved unprocessed meat overnight and added it to the next day’s production. As a result, Hudson recalled more than 25 million pounds of beef, and Burger King severed their business relationship with the meat supplier.
After the crisis, Burger King began a campaign of advertising in newspapers around the country to clear up confusion over whether its beef was safe.
1999 Coleslaw Sickens 11 From Four Outlets of Kentucky Fried Chicken in Ohio

It was a hot summer in southern Ohio. Just after the July 4th holiday, folks who ate tainted coleslaw became sick with symptoms of E. coli. The outbreak sickened 18 people at four Cincinnati locations of Kentucky Fried Chicken; 11 were hospitalized. Ohio health officials noted that it had recorded 30 confirmed cases, and 11 were attributed to KFC. Officials noted particular food-handling errors as possible explanations for the contamination: use of outer cabbage leaves, insufficient washing of cabbage, and use of unpeeled carrots.
The incident changed the way KFC outlets receive and handle coleslaw. No longer was cabbage prepped and chopped at the individual restaurants.
2000’s Meat Contaminates Melon at Sizzler
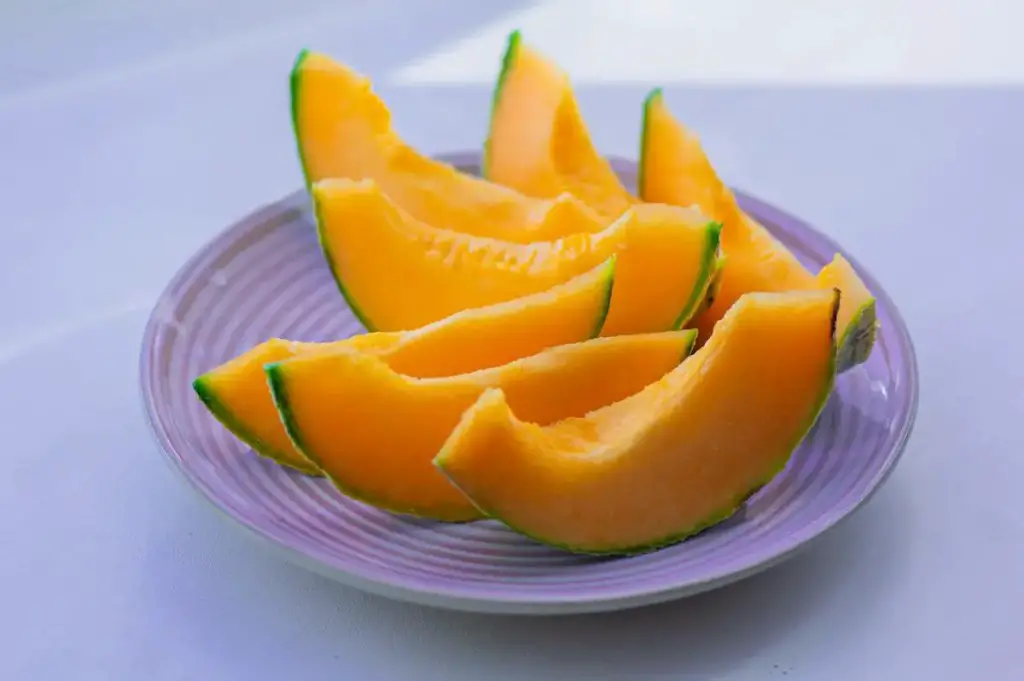
Food handling and facility layout was the culprit at two Sizzler restaurants in Wisconsin. Raw meat for tacos and sirloin tips cross-contaminated watermelon and was the source of an E. coli outbreak in July 2000. This case of restaurant food poisoning resulted in seven hundred thirty-six people falling ill, and 64 cases of E.coli were confirmed. 23 required hospitalization, and a three-year-old girl died. The girl’s family and 138 other plaintiffs reached a $13.5 million settlement with Sizzler’s meat supplier in 2012.
Sizzler struggled to stay alive as a restaurant chain after the outbreak. It emerged from bankruptcy in 1998. It paid families for their medical bills and pursued suits with its suppliers to its credit.
2003 Chi-Chi’s Salsa and Chili Con Queso

The next time you eat green onions, you will remember that they were once the source of the largest outbreak of hepatitis A in the United States. In October 2003, approximately 640 people were affected, including 13 employees. Unfortunately, four died of the illness.
The source was a Chi-Chi’s Tex-Mex restaurant in Monaca, Pennsylvania. The outbreak forced the health department to provide immune globulin vaccinations and post-exposure antibodies to over 9,000 people. This restaurant food poisoning was traced to uncooked green onions used as a garnish. The onions, imported from Mexico, were used in the restaurant’s salsa and chili con queso. However, Chi-Chi’s reputation never recovered. By the following year, the restaurant chain was no longer operating.
2006 Utah Wendy’s e.Coli Contamination

In July 2006, E. coli-contaminated iceberg lettuce was served at a Wendy’s in Utah. The same restaurant served as a caterer during a conference in Utah. At the meeting, the salad was provided, and one individual fell ill with E. coli symptoms. Four persons were taken ill in all. In addition, there were three severe cases of the hemolytic uremic syndrome. This is an E. coli infection that can lead to renal failure.
Taco Bell Makes 71 People Ill in the Northeast in 2006

In December 2006, 71 Taco Bell customers in five northeastern states were sickened with E. coli after eating contaminated shredded lettuce. Taco Bell restaurants where people with the epidemic had eaten are located in New Jersey, New York, Pennsylvania, and Delaware. As a result, eight people suffered kidney failure due to this case of restaurant food poisoning. The cause was determined to be lettuce shipped from California.
This occurrence had a significant influence on the business. Taco Bell’s same-store sales dropped 5%. They fell 11% in the first quarter of 2007. The decline lasted until the third quarter of 2007.
2008, 2013, 2014 Jimmy John’s Sprout Contamination

Jimmy John’s has made headlines with foodborne illnesses in the past ten years. Since 2008, the freshly made from scratch sub sandwich chain served sprouts that resulted in E.coli sickness at least five times. A tally of reports since 2008 shows 479 people affected.
One of the most significant outbreaks of restaurant food poisoning occurred in 2014 when local officials in Michigan, California, Idaho, Montana, Utah, and Washington worked with the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) to investigate an outbreak that affected 19 people in May of 2014. Sprouts were the cause of an outbreak at least five times. In 2013, imported cucumbers from Mexico sickened nine people.
Can I sue a Restaurant For Food Poisoning?
It’s typically not worth the work to file a lawsuit following restaurant food poisoning unless you’ve experienced a life-threatening, severe, long-lasting illness. Those who contract food poisoning and become ill may file a lawsuit against the food’s producer, distributor, and retail outlet. Compensation for damages may include lost wages, medical expenses, and pain and suffering.
You will need to present concrete evidence that you had food poisoning to win the lawsuit based on your testimony alone. Your trip to the doctor is therefore crucial in this regard.
Related Reading
Famous Indiana Foods – We Found 10 Of The Best
A Stealth Review Of The Dark Sky Tavern And Lodge At Port Crescent Mi
14 Outstanding Breakfast Places Near Me To Check Out In Michigan’s Thumb
Sources Consulted – Restaurant Food Poisoning
- Detroit Free Press, Detroit, Michigan, April 4-5, 1977
- Foodborne Illness Outbreak Database via outbreakdatabase.com
- COMPANY NEWS; Jack in the Box’s Worst Nightmare, New York Times 1993
- 10 notable E. coli outbreaks at U.S. fast-food restaurants, UPI, Dec. 31, 2015
- Coleslaw blamed for E. coli outbreak – Cincinnati Enquirer, August 14, 1999
- Wisconsin Sizzlers Vindicated in State Supreme Court, July 12, 2012 – Food Safety News
- Hepatitis A Outbreak Associated with Green Onions at a Restaurant, Morbidity, and Mortality Weekly Report, Centers for Disease Control and Prevention, November 28, 2003
- Salmonella and E. coli Outbreaks: Why Does Jimmy Johns Still Serve Sprouts?, Food Poison Journal, February 2, 2015




